The development of biologics revolutionized the medical industry. Biologics were able to treat several grave conditions, such as inflammatory bowel disease, rheumatoid arthritis, and cancer. However, these therapies have the issue of immunogenicity. Immunogenicity is the development of anti-drug antibodies against protein-based therapies. These issues have plagued several patients and healthcare providers. Despite ongoing safety and tolerability issues in patients, biologics are crucial, particularly for conditions with very limited treatment options.
Long-term treatment with such biologics may be severely affected by anti-drug-antibody (ADA) formation. Therefore, the current article discusses the strategies and challenges around antibody immunogenicity assay, immunogenicity testing methods, PK assays, and assay development for immunogenicity testing of therapeutic proteins. So let us dive deep into immunogenicity testing.
Immunogenicity Testing in Clinical Trials
A significant challenge in using immunogenicity data in clinical and preclinical settings is related to the bioanalytical methods used to assess ADA formation and immune responses. Hence, the FDA has issued guidance titled “Immunogenicity testing of therapeutic protein products.” This material guides in developing and validating bioanalytical assays for ADA detection.
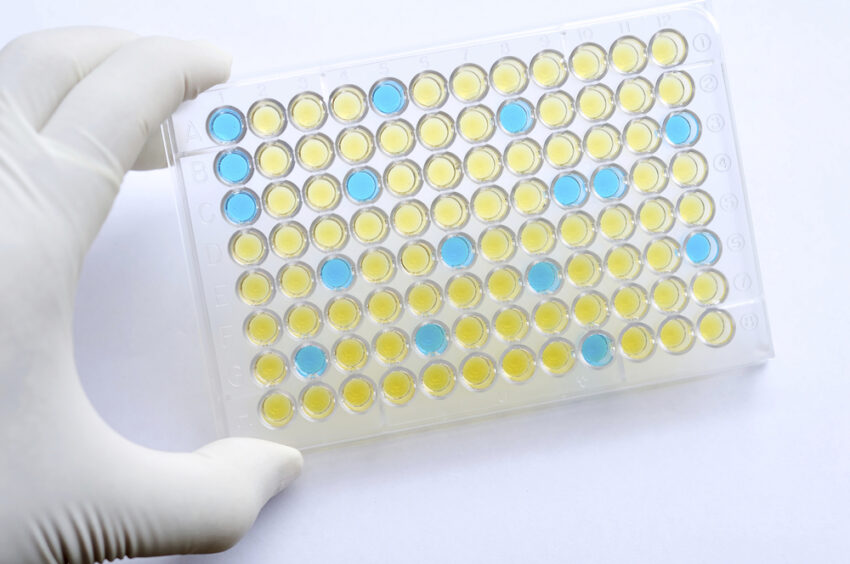
Immunogenicity testing usually follows a three-tier approach. The first tier focuses on assays to minimize false negatives, followed by the next tier of confirmatory assays to reduce false positives. Finally, the last tier consists of assays to characterize various ADAs. Here, the assays focused on the first two tiers of assessment are ligand-binding assays. The major limitation of the ligand-binding assay is the dependence on positive controls for ADAs developed in non-human species. Besides, this response is polyclonal. It will differ from animal to animal and generate ADAs different from those formed in humans. Furthermore, this difference means one may not be able to compare the same therapeutics or different therapeutic proteins when diverse assays are employed. Hence, immunogenicity tests are semiquantitative.
Generally, immunogenicity testing in clinical trials is based on clinical suspicion or drug-level monitoring. Immunoassays are generally the preferred platforms for immunogenicity testing. However, other methods may demonstrate similar performance. For example, one may conduct immunogenicity analysis of anti-TNF biologics through various platforms such as gene-reporter assay, mobility-shift assay, mass spectrometry, or surface plasmon resonance-based assays.
ADA may cause severe consequences, including anaphylaxis, neutralization of life-saving drugs, and cross-reactive antibody-mediated neutralization of endogenous proteins. Hence, preventive strategies are of utmost importance. Not to mention, ADA may cause other intermediary responses, such as complement activation and delayed hypersensitivity responses. Symptoms may include rash, myalgia, arthralgia, fever, hematuria, serositis, proteinuria, and hemolytic anemia.
Also Read: Challenges and Solutions for Good Practices Laboratory-Compliant GLP Labs in the Era of Biologics
There are two primary strategies to mitigate ADA formation. The first option is to induce immune tolerance to therapeutic proteins in clinical development. The second strategy is de-immunizing the protein through predictive algorithms and in vitro approaches. This approach identifies and removes immunogenic epitopes while conserving product activity.
Besides, risk factors not only represent the subsequent consequences but also help identify the probability of generating immune responses. Hence, it is necessary to consider protocol and patient-specific risk factors along with the characteristics of the therapeutic protein to diminish the likelihood of ADA formation.